Allergy and immunology care is essential for individuals suffering from various allergic conditions, which can significantly impact quality of life. With the rising costs of healthcare, finding affordable options is a pressing concern for many patients. This article delves into practical strategies for locating economical allergy and immunology services, including clinic choices, insurance factors, and community resources that can help mitigate financial burdens while ensuring effective treatment.
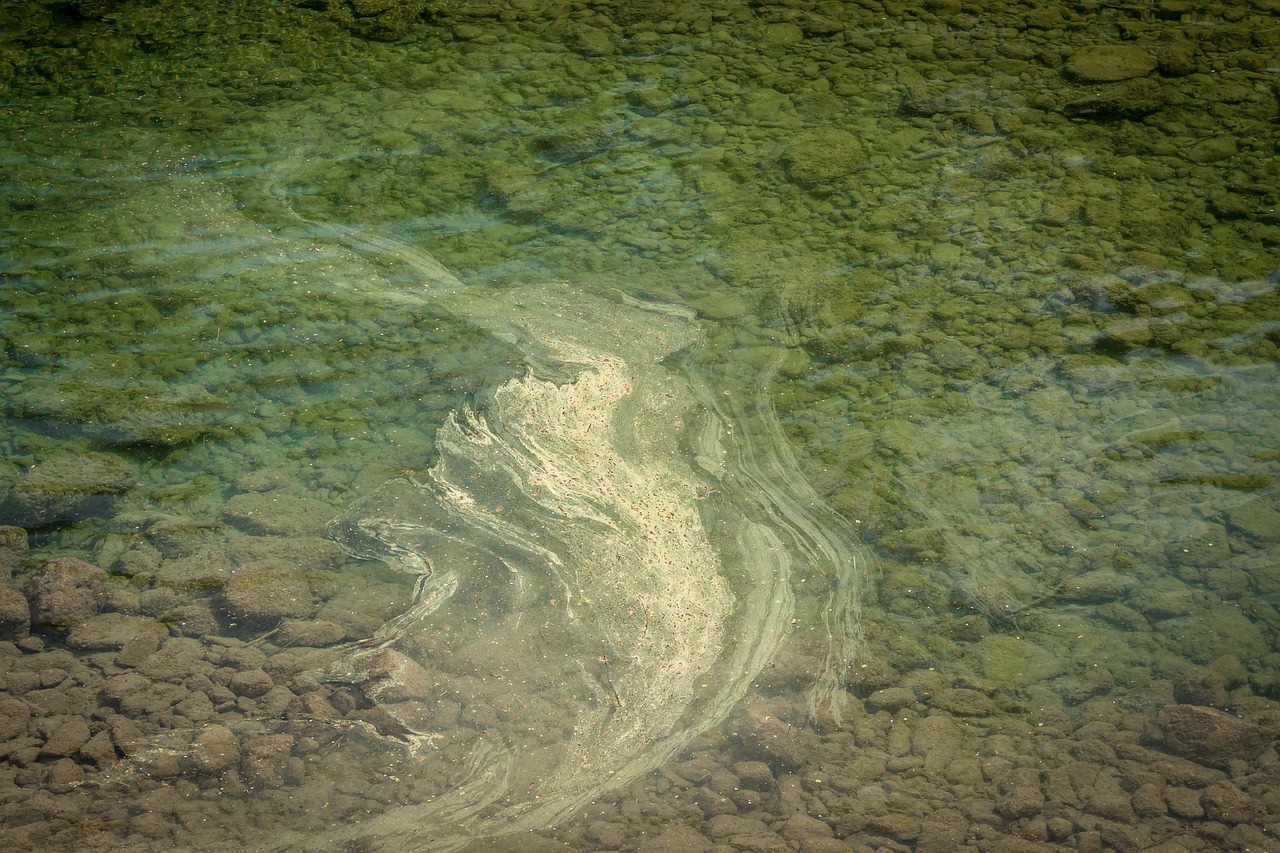
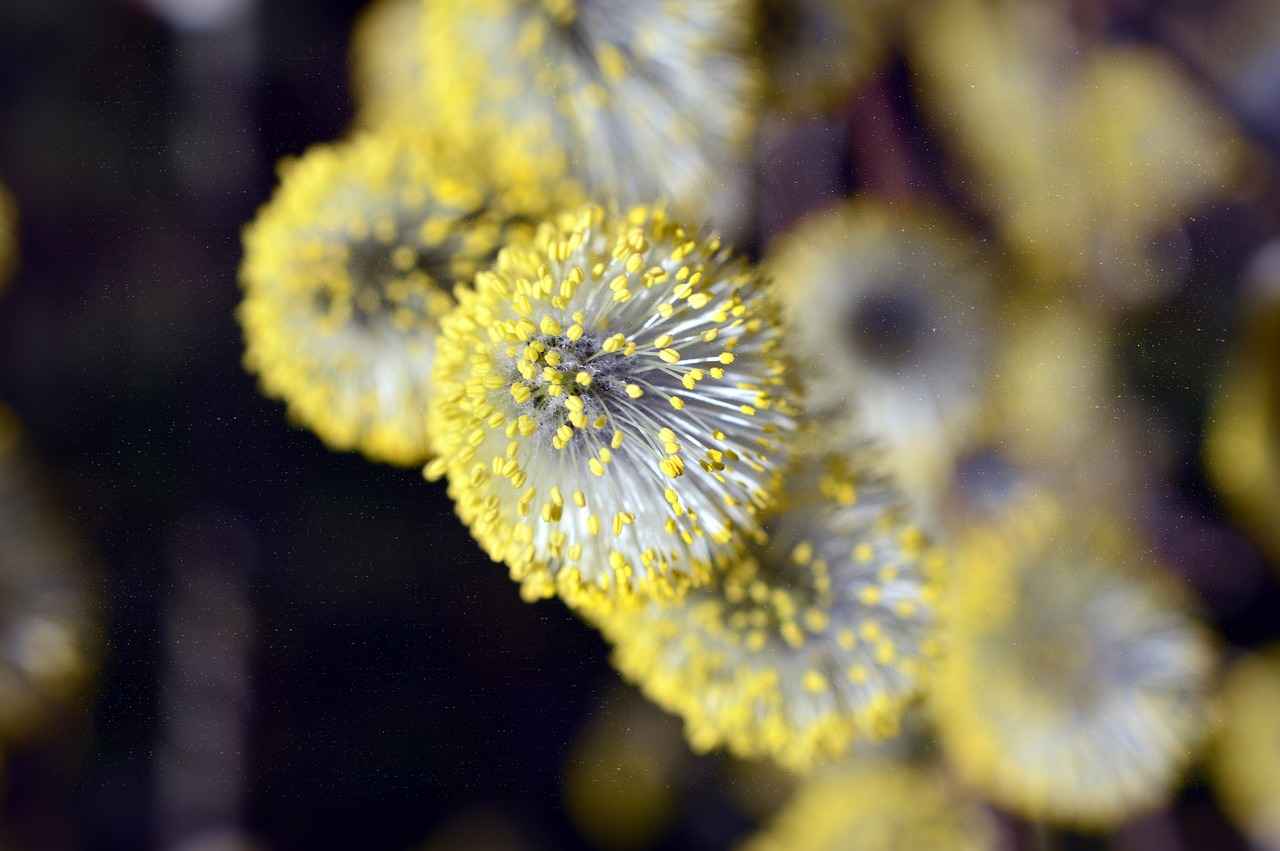
Allergies arise from the immune system’s exaggerated response to specific substances, known as allergens. According to the American Academy of Allergy, Asthma, and Immunology, common allergens include pollen, dust mites, mold, pet dander, and certain foods. Understanding the nature of these allergens is crucial for seeking appropriate care. Immunology, the study of the immune system, encompasses the diagnosis and treatment of allergic reactions, providing insights into the most effective interventions.
Patients have access to a variety of treatment options. Basic strategies involve avoidance of known allergens, but this is not always feasible. Medications such as antihistamines, corticosteroids, and decongestants are frequently prescribed. For example, a study published in the Journal of Allergy and Clinical Immunology highlights how antihistamines can effectively relieve symptoms for many individuals, making them a first-line treatment. However, costs can vary significantly based on brand versus generic options, with generics often providing a more affordable alternative.
| Medication Type | Common Uses | Cost Considerations |
|---|---|---|
| Antihistamines | Relieve sneezing, itching, and runny nose | Generic options are cheaper |
| Corticosteroids | Reduce inflammation | Higher cost, but effective for severe cases |
| Immunotherapy | Long-term desensitization | Initial investment, but potential long-term savings |
For those seeking affordable care, community health centers represent a valuable resource. These centers often offer services on a sliding scale based on income, making them accessible to low-income patients. According to the Health Resources and Services Administration, these centers provide comprehensive care, including allergy treatments, at reduced rates.
Insurance coverage is another critical factor. Patients should thoroughly review their insurance policies, as coverage for allergy treatments can differ widely. Choosing in-network providers typically results in lower costs. Additionally, some plans may require pre-approval or referrals for specialist visits, which can impact overall expenses.
Utilizing online resources can further aid in finding affordable care. Websites that compare clinic prices and services empower patients to make informed choices. Telemedicine has also emerged as a cost-effective alternative, allowing patients to consult with specialists remotely, often at a reduced fee.
Finally, local support groups and nonprofit organizations can provide valuable information and resources, including financial assistance programs. Engaging with community workshops can enhance understanding of allergies and available treatments, leading to better management of conditions.
In conclusion, navigating the landscape of allergy and immunology care requires awareness and proactive measures. By leveraging community resources, understanding treatment options, and utilizing online tools, patients can find affordable care tailored to their specific needs, ensuring that financial constraints do not hinder access to necessary treatments.

Understanding Allergies and Immunology
is essential for anyone dealing with allergic reactions or seeking effective treatment options. Allergies occur when the immune system reacts abnormally to substances known as allergens, which can include pollen, dust mites, certain foods, and pet dander. This hypersensitivity can lead to a variety of symptoms, ranging from mild irritations like sneezing and itching to severe reactions, such as anaphylaxis. On the other hand, immunology is the branch of medicine that focuses on the immune system, its functions, and its disorders. By comprehending these concepts, patients can better navigate their treatment options and identify suitable clinics for their needs.
Allergic reactions are mediated by the immune system’s response to what it mistakenly perceives as harmful. For instance, when a person with a pollen allergy breathes in pollen, their immune system produces antibodies that trigger the release of histamines, leading to symptoms such as nasal congestion and itchy eyes. According to a study published in the Journal of Allergy and Clinical Immunology, approximately 30% of adults and 40% of children in the United States are affected by allergies, highlighting the widespread nature of this condition.
Understanding the immune system’s functioning is crucial for developing effective treatments. Immunologists study various aspects of the immune response, including how it can be modified or enhanced. For example, immunotherapy, which is often used in treating allergies, involves gradually exposing patients to increasing amounts of an allergen to build tolerance. Research has shown that this method can lead to long-term relief from allergic symptoms, as evidenced by findings from the American Academy of Allergy, Asthma & Immunology.
Furthermore, understanding the connection between allergies and the immune system can help patients make informed decisions regarding their treatment options. Patients should be aware of the various types of treatments available, such as antihistamines, which are commonly used to alleviate symptoms, and corticosteroids, which can reduce inflammation. Knowing the differences among these treatments, their costs, and how they interact with individual health conditions is vital for effective management.
- Antihistamines: Block the action of histamine and provide quick relief from symptoms.
- Corticosteroids: Help reduce inflammation and are often used in nasal sprays.
- Immunotherapy: A long-term treatment option that can lead to lasting symptom relief.
In summary, a comprehensive understanding of allergies and immunology is critical for patients seeking effective care. By grasping how these concepts interrelate, individuals can better navigate treatment options and find clinics that meet their specific needs. This knowledge empowers patients to take control of their health and make informed decisions about their allergy management.

Types of Allergy Treatments Available
Allergies affect millions of individuals worldwide, leading to discomfort and, in some cases, severe health issues. Effective management of allergies is crucial for improving quality of life. The landscape of allergy treatments is diverse, encompassing a range of approaches from simple avoidance strategies to advanced medical interventions. Understanding these treatment modalities is essential for patients seeking relief from their symptoms.
Allergy avoidance is often the first line of defense. This strategy involves identifying and steering clear of allergens, such as pollen, dust mites, pet dander, and certain foods. For instance, individuals with pollen allergies might benefit from staying indoors during high pollen seasons and using air purifiers. In contrast, those allergic to specific foods need to read labels carefully and avoid cross-contamination in food preparation.
When avoidance is not feasible or sufficient, medications come into play. Antihistamines are among the most commonly prescribed drugs for allergies. They work by blocking histamine, a chemical released during an allergic reaction, thereby alleviating symptoms like sneezing, itching, and runny nose. A study published in the Journal of Allergy and Clinical Immunology demonstrated that both first-generation and second-generation antihistamines are effective, although the latter tend to have fewer sedative effects, making them preferable for daytime use.
Corticosteroids are another category of medications that reduce inflammation associated with allergic reactions. These can be administered as nasal sprays, inhalers, or oral tablets, depending on the severity of the symptoms. Research indicates that intranasal corticosteroids are particularly effective for allergic rhinitis, providing significant relief and improving overall nasal function.
For those seeking long-term solutions, immunotherapy presents a compelling option. This treatment involves gradually exposing patients to allergens, either through injections (allergy shots) or sublingual tablets, to build tolerance. A meta-analysis in The Cochrane Database of Systematic Reviews highlighted that immunotherapy can lead to lasting symptom relief even after treatment has concluded, making it a valuable investment in long-term health.
In addition to these conventional treatments, some patients explore alternative therapies such as acupuncture or herbal remedies. While anecdotal evidence supports their efficacy, scientific validation remains limited. Therefore, patients should approach these options with caution and consult healthcare professionals before integrating them into their treatment plans.
Ultimately, the choice of allergy treatment should be guided by a thorough understanding of individual needs, preferences, and medical history. By collaborating with healthcare providers and considering all available options, patients can develop a comprehensive strategy to manage their allergies effectively.
Medications for Allergies
Medications for allergies play a crucial role in managing symptoms and improving the quality of life for millions of individuals. Among the most commonly prescribed medications are antihistamines, corticosteroids, and decongestants. Each category of medication serves distinct purposes and has varying costs, which can significantly influence overall treatment expenses.
Antihistamines are often the first line of defense against allergy symptoms. They work by blocking the action of histamine, a chemical released during allergic reactions. This action helps alleviate symptoms such as sneezing, itching, and runny nose. There are two main types of antihistamines: first-generation and second-generation. First-generation antihistamines, like diphenhydramine (Benadryl), can cause drowsiness, while second-generation options, such as cetirizine (Zyrtec) and loratadine (Claritin), are less sedating and more suitable for daytime use. The cost of these medications can vary widely; generic versions are typically more affordable than their brand-name counterparts, making them accessible for many patients.
Corticosteroids, including nasal sprays like fluticasone (Flonase) and budesonide (Rhinocort), are effective in reducing inflammation associated with allergic rhinitis. These medications are particularly beneficial for individuals with persistent symptoms, as they address the underlying inflammation rather than just the symptoms. While corticosteroids may involve higher upfront costs, their long-term effectiveness can lead to reduced need for additional medications, ultimately lowering overall treatment expenses.
Decongestants, such as pseudoephedrine (Sudafed), are another option for allergy relief. They work by constricting blood vessels in the nasal passages, reducing swelling and congestion. However, decongestants are not recommended for prolonged use due to potential side effects, including increased blood pressure and insomnia. Patients should consider the cost of decongestants, especially if they require frequent use, as this can add up over time.
In addition to these medications, it is essential for patients to be aware of potential interactions and side effects. Consulting with healthcare professionals can provide personalized recommendations based on individual health profiles. Moreover, understanding the financial implications of different medications can empower patients to make informed choices about their treatment plans.
In summary, the choice of allergy medications—antihistamines, corticosteroids, and decongestants—depends on specific symptoms, individual health conditions, and financial considerations. By evaluating these factors, patients can optimize their allergy management strategies, ensuring effective treatment while minimizing costs.
Antihistamines
are a cornerstone in the management of allergic reactions, providing relief from symptoms such as sneezing, itching, and nasal congestion. These medications function by blocking the action of histamine, a chemical released by the immune system during an allergic reaction. By inhibiting histamine’s effects on the body, antihistamines significantly reduce the intensity of allergy symptoms, allowing individuals to maintain their quality of life despite exposure to allergens.
There are two main categories of antihistamines: first-generation and second-generation. First-generation antihistamines, such as diphenhydramine (Benadryl), are known for their sedative effects, which can be beneficial for individuals who experience insomnia due to allergy symptoms. However, their sedative properties can also lead to drowsiness, making them less suitable for daytime use. In contrast, second-generation antihistamines, including cetirizine (Zyrtec) and loratadine (Claritin), are designed to minimize sedation while effectively alleviating allergy symptoms. This makes them a popular choice for those needing relief during daily activities.
Cost is a significant factor in medication selection, and many patients find that generic antihistamines offer a more affordable alternative to their brand-name counterparts. For example, while a brand-name medication may retail at a higher price, its generic version can provide the same active ingredients and efficacy at a fraction of the cost. This affordability is particularly important for individuals with chronic allergies who require ongoing treatment.
Research supports the effectiveness of antihistamines in managing allergic rhinitis, with studies indicating that these medications can improve overall quality of life for allergy sufferers. A systematic review published in the Journal of Allergy and Clinical Immunology highlighted that both first and second-generation antihistamines significantly reduce symptoms and improve sleep quality in patients with seasonal allergies.
While antihistamines are effective, they are not the only treatment option available. Patients may also consider immunotherapy, which involves gradually exposing the immune system to allergens to build tolerance. Though this approach may have a higher initial cost, it can lead to long-term relief and potentially reduce the need for medication over time.
In conclusion, antihistamines play a vital role in the management of allergy symptoms by blocking histamine and providing relief. With the availability of both brand-name and generic options, patients can choose cost-effective solutions that suit their needs. As with any medication, it is advisable to consult healthcare professionals to determine the best treatment plan tailored to individual circumstances.
Immunotherapy Options
Immunotherapy represents a significant advancement in the treatment of allergies, specifically through methods such as allergy shots (subcutaneous immunotherapy) and sublingual tablets (sublingual immunotherapy). These therapies aim to gradually desensitize patients to specific allergens, effectively retraining the immune system to respond more appropriately to these triggers.
The process of immunotherapy involves the administration of controlled doses of allergens, which are progressively increased over time. This gradual exposure helps the immune system build tolerance. For instance, a study published in the *Journal of Allergy and Clinical Immunology* found that patients receiving subcutaneous immunotherapy for pollen allergies experienced a significant reduction in symptoms and medication use after three years of treatment.
While the initial costs of immunotherapy can be higher compared to traditional allergy medications, such as antihistamines or corticosteroids, the long-term benefits often outweigh these expenses. According to research from the *American Academy of Allergy, Asthma & Immunology*, patients who undergo immunotherapy may experience lasting relief from allergy symptoms even after treatment has concluded. This long-term efficacy can lead to reduced healthcare costs over time, as fewer medications and doctor visits are required.
To provide a clearer understanding of the financial implications, consider the following comparison:
| Treatment Type | Initial Cost (Approx.) | Long-term Cost Savings |
|---|---|---|
| Allergy Shots | $1,500 – $3,000/year | Up to 50% reduction in symptom-related costs over 5 years |
| Sublingual Tablets | $600 – $1,200/year | Similar savings as allergy shots with potentially fewer side effects |
| Traditional Medications | $300 – $1,000/year | Ongoing costs without long-term relief |
In addition to cost considerations, the choice between allergy shots and sublingual tablets may also depend on patient preference and lifestyle. Allergy shots require regular visits to an allergist, which may be inconvenient for some individuals. In contrast, sublingual tablets can be taken at home, providing a more flexible option for many patients.
Ultimately, immunotherapy is a viable and effective treatment option for those suffering from allergies. Despite the initial financial investment, the potential for long-term relief and reduced healthcare costs makes it a compelling choice for many patients. As always, individuals should consult with healthcare professionals to determine the most appropriate treatment plan tailored to their specific needs.
Alternative Treatments
for allergies, including herbal remedies and acupuncture, have gained popularity as adjuncts to traditional medical approaches. While some patients report positive outcomes, it is essential to critically assess the efficacy and safety of these alternatives in comparison to established treatments.
Herbal remedies, such as butterbur and quercetin, have been studied for their potential to alleviate allergy symptoms. Research indicates that butterbur may be as effective as antihistamines for treating hay fever, with fewer side effects. A study published in the Journal of Allergy and Clinical Immunology found that patients taking butterbur experienced significant symptom relief without the sedation commonly associated with traditional medications. However, the quality and concentration of herbal products can vary widely, raising concerns about standardization and dosage.
Acupuncture, another alternative treatment, is often sought for its potential to reduce allergic reactions. Some studies suggest that acupuncture may help alleviate symptoms by modulating the immune response. A meta-analysis in the American Journal of Rhinology & Allergy concluded that acupuncture could significantly improve nasal symptoms in allergic rhinitis patients. Nonetheless, the mechanism behind these effects remains poorly understood, and more rigorous clinical trials are needed to establish its reliability and safety.
It is crucial for patients considering alternative treatments to consult healthcare professionals, particularly allergists or immunologists, to discuss potential interactions with conventional medications. The integration of alternative therapies should be approached cautiously, as some herbal remedies can interfere with prescribed treatments or exacerbate conditions.
Furthermore, the regulatory landscape surrounding alternative treatments differs significantly from that of conventional medicine. In many countries, herbal supplements are not subject to the same rigorous testing and approval processes as pharmaceuticals. This lack of oversight can lead to discrepancies in product quality and patient safety, making it essential for consumers to choose reputable brands and consult with knowledgeable practitioners.
In summary, while alternative treatments such as herbal remedies and acupuncture may offer relief for some allergy sufferers, their efficacy and safety must be carefully weighed against traditional options. Patients should remain informed and consult healthcare providers to ensure a comprehensive approach to allergy management that prioritizes both effectiveness and safety.
Finding Affordable Clinics
Finding affordable clinics for allergy treatment is a crucial step for individuals seeking effective care without overwhelming financial burdens. Identifying low-cost allergy clinics necessitates a thorough understanding of available resources and options. Community health centers, which often provide services based on income, and clinics with sliding-scale fee structures are vital components of this search.
Community health centers are designed to offer comprehensive care to underserved populations. These centers frequently provide allergy services at significantly reduced rates. For instance, a study published in the Journal of Community Health found that community health centers can reduce healthcare costs by up to 40% for low-income patients. They often employ a model that assesses a patient’s ability to pay, ensuring that those in financial need receive necessary treatments without incurring crippling debt.
In addition to community health centers, many clinics offer sliding scale fees. This pricing model adjusts the cost of services based on a patient’s income and family size. For example, a patient earning below a certain threshold may pay a nominal fee for consultations and treatments, while those with higher incomes may pay a more standard rate. This flexible pricing structure is essential for ensuring that allergy care remains accessible to all, regardless of financial status.
Moreover, it is important for patients to be proactive in their search for affordable care. Utilizing online resources such as HealthCare.gov can help individuals locate clinics that fit their financial needs. These platforms often provide comprehensive lists of services, including patient reviews and cost estimates, which can significantly aid in decision-making.
Another avenue worth exploring is the possibility of nonprofit organizations that focus on allergy awareness and support. These organizations frequently provide financial assistance programs and can guide patients toward resources that might not be immediately apparent. For example, the Asthma and Allergy Foundation of America offers a wealth of information, including directories of affordable care options.
In conclusion, navigating the landscape of allergy treatment requires diligence and resourcefulness. By leveraging community health centers, sliding-scale fee structures, and online resources, patients can find affordable clinics that meet their needs. Understanding these options not only helps in accessing necessary care but also empowers individuals to make informed decisions regarding their health.
Community Health Centers
play a pivotal role in providing accessible healthcare services, particularly for individuals facing financial challenges. These centers are designed to cater to the health needs of underserved populations, offering a range of services, including allergy care at reduced rates. By focusing on a sliding scale fee structure, they ensure that patients only pay what they can afford, making essential treatments more attainable.
One of the significant advantages of community health centers is their focus on comprehensive care. Unlike traditional clinics that may specialize in specific areas, these centers often provide a holistic approach to health, addressing not only allergies but also general health concerns, chronic disease management, and preventive care. For instance, a patient experiencing allergic reactions may also receive education on lifestyle changes and environmental factors that contribute to their condition, thus receiving a more rounded approach to their health.
Research indicates that low-income patients are disproportionately affected by allergies and related conditions. According to a study published in the Journal of Allergy and Clinical Immunology, individuals in lower socioeconomic brackets are more likely to experience severe allergic reactions due to limited access to preventive care and medications. Community health centers address this disparity by offering tailored allergy services that take into account a patient’s income level, ensuring that they receive the care they need without financial strain.
Furthermore, community health centers often collaborate with local organizations to enhance their services. For example, some centers partner with universities to conduct research on allergy prevalence in specific demographics, which in turn informs their treatment protocols. This collaborative approach not only improves patient outcomes but also contributes to the broader understanding of allergic conditions within the community.
In addition to direct care, community health centers provide educational resources on managing allergies effectively. Workshops and seminars are frequently organized to inform patients about the importance of recognizing triggers, understanding treatment options, and utilizing available resources. This empowerment through education is crucial for patients who may feel overwhelmed by their conditions.
In conclusion, community health centers are invaluable resources for low-income patients seeking allergy care. By offering comprehensive services at reduced rates, they not only address immediate health concerns but also contribute to long-term wellness through education and preventive measures. As healthcare continues to evolve, the role of these centers remains essential in fostering equitable access to quality care.
Sliding Scale Fees
are an innovative approach adopted by many healthcare clinics to ensure that patients receive necessary medical care without facing overwhelming financial burdens. This fee structure adjusts the cost of services based on an individual’s income and financial situation, making healthcare more accessible to those who might otherwise forgo treatment due to cost concerns.
For instance, clinics that implement sliding scale fees typically assess a patient’s income, family size, and overall financial situation to determine an affordable rate for services. This model is particularly beneficial for low-income individuals or families who may struggle to pay standard rates for allergy treatments, which can include consultations, diagnostic tests, and ongoing therapies.
Research indicates that patients who utilize sliding scale clinics often experience significantly reduced out-of-pocket expenses. A study published in the American Journal of Public Health found that patients at sliding scale clinics reported a 30% reduction in healthcare costs compared to those at traditional practices. This reduction can facilitate timely access to essential allergy treatments, such as immunotherapy or medication, which are critical for managing conditions like asthma, allergic rhinitis, and eczema.
Additionally, sliding scale clinics often provide a range of services beyond allergy treatments. Many integrate primary care, mental health services, and preventive care, allowing patients to address multiple health concerns in one location. This holistic approach not only enhances patient care but also encourages individuals to seek help before conditions worsen, ultimately leading to better health outcomes.
Moreover, sliding scale fees can help alleviate the financial strain on community health systems. By ensuring that low-income patients receive necessary care, clinics can reduce the incidence of emergency room visits, which are often more costly and less effective for managing chronic conditions like allergies.
- Benefits of Sliding Scale Fees:
- Increased access to necessary treatments.
- Reduced financial barriers for low-income patients.
- Comprehensive care options available in one location.
- Potential for improved health outcomes through timely interventions.
In conclusion, sliding scale fee structures represent a vital resource for individuals seeking affordable allergy care. By adjusting costs based on income, these clinics not only provide essential treatments but also promote health equity within communities. Patients are encouraged to research local clinics that offer this payment model to ensure they can access the care they need without incurring significant financial hardship.

Insurance Coverage for Allergy Care
is a critical factor that influences both access to treatment and overall healthcare costs. As allergies become increasingly prevalent, understanding the nuances of insurance policies can significantly impact patients’ financial responsibilities and treatment choices. Coverage for allergy treatments often varies widely among different insurance plans, making it essential for patients to navigate these complexities effectively.
Many insurance policies provide coverage for a range of allergy treatments, including medications, immunotherapy, and diagnostic tests. However, the extent of this coverage can differ greatly. For instance, while some plans may fully cover the cost of allergy testing and routine medications like antihistamines, others may impose significant out-of-pocket expenses for these services. A study published in the Journal of Allergy and Clinical Immunology found that nearly 30% of patients faced unexpected costs due to inadequate insurance coverage for essential allergy treatments.
Understanding the difference between in-network and out-of-network providers is also crucial. In-network providers typically have negotiated rates with insurance companies, resulting in lower costs for patients. Conversely, seeing an out-of-network provider can lead to much higher expenses. According to the American Academy of Allergy, Asthma & Immunology, patients can save an average of 40% on their total healthcare costs by choosing in-network specialists.
Moreover, some insurance plans require pre-approval or referrals for specialist visits. This can complicate the process of accessing timely care, particularly for patients experiencing severe allergic reactions. A survey conducted by the National Institute of Allergy and Infectious Diseases revealed that patients who understood their insurance requirements were 50% more likely to receive timely treatment compared to those who did not.
- Key Considerations for Patients:
- Review your insurance policy to understand the specifics of allergy treatment coverage.
- Contact your insurance provider to clarify any questions regarding in-network and out-of-network benefits.
- Keep track of any pre-approval requirements to avoid unexpected denials of coverage.
In addition to traditional insurance coverage, patients may explore health savings accounts (HSAs) or flexible spending accounts (FSAs) as potential ways to offset the costs of allergy treatments. These accounts allow individuals to set aside pre-tax dollars for medical expenses, providing a financial cushion for out-of-pocket costs.
In conclusion, navigating the complexities of insurance coverage for allergy care requires diligence and informed decision-making. By understanding the specifics of their insurance plans, patients can minimize their financial burden while ensuring they receive the necessary treatments for their allergies. As the landscape of healthcare continues to evolve, staying informed about insurance options will empower patients to make better choices for their health.
In-Network vs. Out-of-Network Providers
When it comes to managing healthcare costs, understanding the difference between in-network and out-of-network providers is crucial. In-network providers are those who have established contracts with your health insurance company, allowing for negotiated rates that generally result in lower out-of-pocket expenses for patients. In contrast, out-of-network providers do not have such agreements, which can lead to significantly higher costs for services rendered.
Choosing in-network providers typically results in lower costs due to these negotiated rates. For instance, a recent study published in the Journal of Health Economics found that patients who utilized in-network services experienced an average savings of 30% compared to those who sought care from out-of-network providers. This difference can be substantial, especially for patients requiring ongoing treatment for chronic conditions such as allergies or asthma.
It is essential for patients to verify which clinics are covered under their insurance plans to avoid unexpected bills. Insurance companies typically provide a directory of in-network providers on their websites, which can be a valuable resource for patients. Additionally, contacting the insurance company directly can clarify any uncertainties regarding coverage. For example, a patient might discover that a nearby allergy clinic is in-network, which could save them hundreds of dollars in treatment costs.
Furthermore, understanding the implications of out-of-network care is equally important. Patients who choose to see an out-of-network provider may face higher deductibles and co-pays, or even find that their insurance does not cover the service at all. This lack of coverage can lead to financial strain, particularly for those who require frequent visits or specialized treatments.
To illustrate this point, consider a patient with severe allergies who opts for an out-of-network specialist. If the total cost of an allergy consultation is $200, and the insurance plan covers only 50% for out-of-network services, the patient would be responsible for $100. In contrast, if the same patient had chosen an in-network provider with a negotiated rate of $120, their out-of-pocket cost would be just $20, highlighting the importance of making informed choices.
Additionally, some insurance plans may require pre-approval or referrals for specialist visits, which can further complicate access to care. Patients should familiarize themselves with their insurance policies to navigate these requirements effectively. By doing so, they can avoid unnecessary delays in receiving treatment and ensure they are maximizing their insurance benefits.
In conclusion, selecting in-network providers is a strategic way to minimize healthcare costs. Patients should actively engage with their insurance plans, verify coverage, and understand the financial implications of their healthcare choices. By making informed decisions, patients can secure the necessary care while maintaining financial stability.
Pre-Approval and Referrals
In the realm of healthcare, understanding the nuances of insurance plans is crucial for patients seeking specialized care. Pre-approval and referrals are terms that often surface in discussions about insurance coverage, particularly when it comes to visiting specialists in fields like allergy and immunology. These requirements can significantly influence a patient’s access to necessary treatments and consultations.
Many insurance plans stipulate that patients must obtain pre-approval before seeing a specialist. This means that the primary care physician (PCP) must evaluate the patient’s condition and determine if a referral to a specialist is warranted. For instance, a patient experiencing severe allergic reactions may need to see an allergist. If their insurance requires pre-approval, the PCP must submit documentation justifying the need for specialist intervention. This process can be time-consuming and may delay essential care.
Research indicates that understanding these insurance requirements can lead to more effective navigation of healthcare systems. A study published in the Journal of Health Economics found that patients who are well-informed about their insurance policies are more likely to receive timely care and avoid unnecessary out-of-pocket expenses. Patients should take the initiative to understand their plan’s specifics, including whether pre-approval is needed for specialist visits and how to initiate the referral process.
- Check Your Insurance Policy: Review the details of your insurance plan to identify any requirements for referrals or pre-approval.
- Consult Your PCP: Discuss your symptoms and concerns with your primary care physician, who can guide you on the referral process.
- Document Everything: Keep records of all communications and submissions related to pre-approval to ensure a smooth transition to specialist care.
Furthermore, failure to adhere to these pre-approval processes can result in claims being denied, leaving patients with unexpected medical bills. According to the American Journal of Managed Care, nearly 30% of claims for specialist visits are denied due to lack of necessary pre-approval. This statistic underscores the importance of understanding and following your insurance plan’s protocols.
In some cases, patients may find that their insurance plan allows for direct access to certain specialists without a referral. However, this varies widely among different insurance providers and plans. Thus, it is essential for patients to clarify these details with their insurance representatives.
In conclusion, navigating the complexities of insurance requirements, such as pre-approval and referrals, is a critical skill for patients seeking specialized care. By being proactive and informed, patients can ensure they receive timely and necessary treatment without facing unnecessary financial burdens.
Utilizing Online Resources
In today’s digital age, online resources have become invaluable tools for patients seeking affordable allergy care. With the rise of numerous health-focused websites, individuals can now easily compare clinic services and prices, ensuring they make informed decisions about their healthcare options.
One of the most effective ways to locate budget-friendly allergy clinics is through specialized websites that aggregate information about various healthcare providers. These platforms not only display clinic prices but also provide patient reviews and ratings, helping users gauge the quality of care offered. For instance, sites like Healthgrades and Yelp enable patients to read firsthand accounts of others’ experiences, which can be crucial in selecting a reliable clinic.
Furthermore, many of these websites feature price comparison tools that allow patients to evaluate the costs associated with different treatment options. This transparency empowers patients to choose clinics that not only fit their budget but also meet their healthcare needs. Research indicates that patients who actively engage in price comparison are more likely to find affordable care, ultimately leading to better health outcomes.
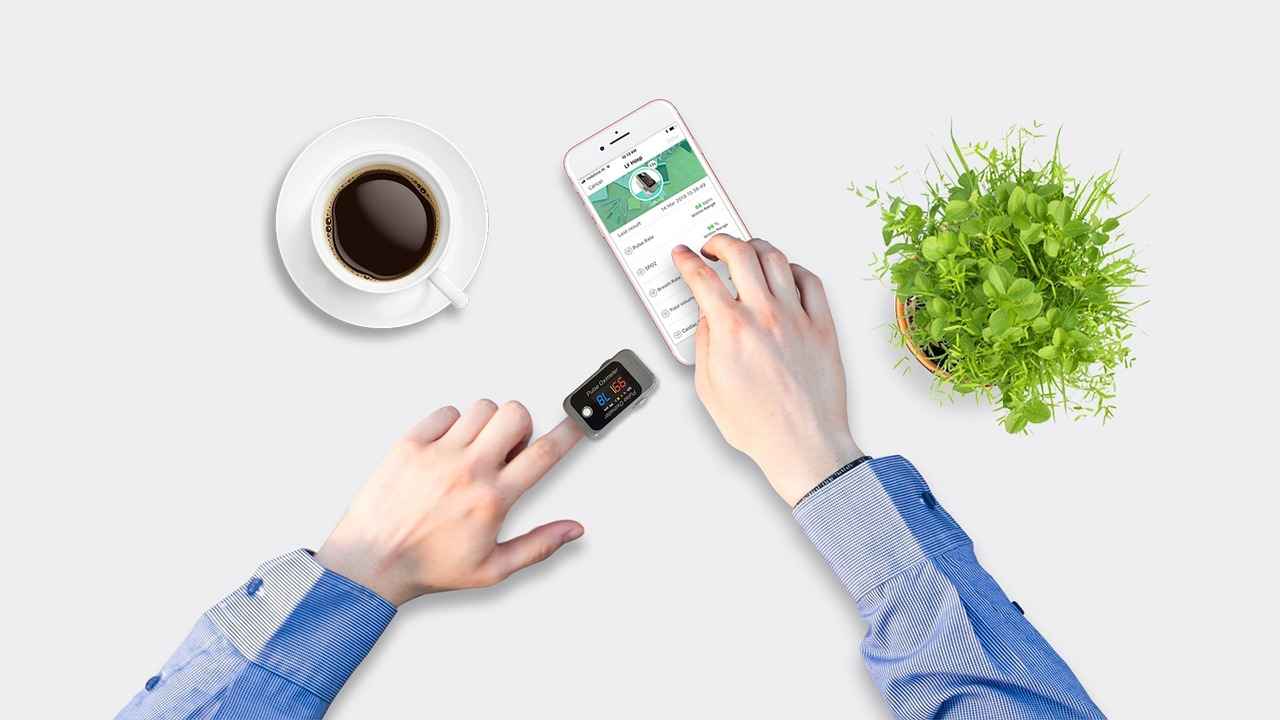
Another significant advantage of utilizing online resources is the availability of telemedicine services. Telemedicine has revolutionized access to allergy specialists, offering consultations at a fraction of the cost of traditional in-person visits. Patients can connect with healthcare providers from the comfort of their homes, which is particularly beneficial for those in remote areas or with mobility issues. Studies have shown that telemedicine can reduce healthcare costs while maintaining a high standard of care, making it an attractive option for many.
Additionally, online platforms often provide educational resources about various allergy treatments, including medications and alternative therapies. This information can help patients understand their options better and engage in discussions with their healthcare providers. For example, a patient might learn about the effectiveness of immunotherapy versus over-the-counter medications, enabling them to make more informed choices regarding their treatment plans.
Moreover, many local health organizations and nonprofits maintain websites that offer information about community resources, workshops, and financial assistance programs. These resources can be critical for low-income patients who may struggle to afford necessary treatments. By connecting with local support groups through online platforms, patients can gain insights and recommendations based on shared experiences, enhancing their ability to navigate the healthcare system effectively.
In conclusion, leveraging online resources is essential for patients seeking affordable allergy care. By utilizing price comparison tools, accessing telemedicine services, and engaging with educational materials, individuals can make informed decisions that prioritize their health without compromising their financial well-being.
Telemedicine Options
Telemedicine has revolutionized the way patients access healthcare services, particularly in the fields of allergy and immunology. This innovative approach allows patients to consult with specialists from the comfort of their homes, significantly reducing the need for in-person visits. The convenience of telemedicine not only enhances patient satisfaction but also offers a cost-effective solution for those seeking specialized care.
Research indicates that telemedicine consultations can be up to 30% cheaper than traditional in-person visits. A study published in the Journal of Allergy and Clinical Immunology found that patients utilizing telehealth services reported lower overall costs associated with travel, time off work, and direct medical fees. This is particularly beneficial for individuals living in rural or underserved areas, where access to allergists may be limited.
Moreover, telemedicine platforms often provide a range of services, including video consultations, electronic prescriptions, and remote monitoring of symptoms. For instance, patients with chronic allergies can engage in regular follow-ups without the burden of traveling long distances. This not only saves money but also ensures that patients receive timely adjustments to their treatment plans based on real-time feedback.
In addition to cost savings, telemedicine facilitates immediate access to specialists. Patients experiencing acute allergic reactions can quickly consult with an allergist, receive guidance on managing their symptoms, and obtain prescriptions if necessary. A study by the American Academy of Allergy, Asthma & Immunology highlights that telemedicine significantly reduces wait times for appointments, allowing for quicker interventions that can prevent complications.
However, it is essential to consider some limitations of telemedicine. Not all conditions can be adequately assessed without a physical examination, and some patients may require diagnostic tests that necessitate in-person visits. Therefore, a hybrid approach that combines telemedicine with traditional care may be the most effective strategy for comprehensive allergy management.
To maximize the benefits of telemedicine, patients should ensure that their chosen provider is board-certified and has experience in allergy and immunology. Additionally, checking for insurance coverage for telehealth services can further enhance affordability. Many insurance plans now include telemedicine as part of their coverage, reflecting a growing acceptance of this mode of healthcare delivery.
In conclusion, telemedicine is not just a temporary solution but a sustainable alternative that enhances access to allergy and immunology care. By leveraging this technology, patients can enjoy affordable and convenient healthcare, paving the way for better health outcomes and improved quality of life.
Patient Reviews and Ratings
serve as a vital resource for individuals seeking to make informed decisions about their healthcare providers, particularly in the field of allergy and immunology. These reviews can reveal essential insights into the quality of care, patient satisfaction, and the overall affordability of services offered by various clinics and hospitals.
Websites such as Healthgrades and Yelp are invaluable tools for patients looking to evaluate potential healthcare providers. By aggregating patient feedback, these platforms allow prospective patients to gauge the reputation and reliability of clinics based on real experiences. For instance, a study published in the Journal of Medical Internet Research highlights that patient reviews significantly impact the selection of healthcare providers, with many individuals prioritizing providers with higher ratings and positive feedback.
Moreover, understanding the context behind these reviews is crucial. Patients often share their experiences regarding wait times, the demeanor of healthcare staff, and the effectiveness of treatments received. A clinic that consistently receives positive reviews for its attentive staff and efficient service may indicate a higher likelihood of patient satisfaction. Conversely, recurring complaints about long wait times or unresponsive staff could suggest underlying issues that potential patients should consider.
In addition to quality of care, affordability is a significant factor in healthcare decisions. Many patients report their experiences regarding the costs associated with treatments and services. For example, a user review may mention that a particular clinic offers competitive pricing for allergy testing compared to other local providers. This kind of information is invaluable for those navigating the often-complex landscape of healthcare costs.
Furthermore, the accessibility of these reviews allows patients to compare multiple providers quickly. By analyzing ratings and reading through various testimonials, individuals can create a shortlist of clinics that meet their needs both financially and in terms of quality of care. This process not only empowers patients but also encourages clinics to maintain high standards of service to attract and retain clientele.
In conclusion, patient reviews and ratings are essential components in the decision-making process for allergy and immunology care. They provide a wealth of information that can guide patients towards reputable providers while highlighting cost-effective options. By utilizing platforms like Healthgrades and Yelp, patients can make informed choices that lead to better health outcomes and increased satisfaction with their healthcare experience.

Local Support Groups and Resources
Local support groups play a crucial role in the landscape of allergy care, offering valuable information and resources for patients who are navigating the challenges of managing their allergies. These groups often consist of individuals who share similar experiences and can provide insights that are both practical and empathetic. For many patients, the journey to finding affordable allergy care can be daunting, and connecting with others who have faced similar hurdles can be immensely beneficial.
Support groups can facilitate shared experiences that lead to recommendations for local clinics, specialists, and treatment options. For instance, members may share their experiences with various healthcare providers, detailing the costs associated with different treatments and the effectiveness of those treatments. This collective knowledge can help patients make informed decisions about where to seek care.
In addition to personal recommendations, local support groups often collaborate with healthcare professionals to host educational workshops and seminars. These events can cover a range of topics, from understanding allergy triggers to exploring the latest treatment options. Such workshops not only enhance patients’ knowledge but also empower them to advocate for their health needs effectively.
Moreover, many support groups maintain a network of resources that include information on financial assistance programs, sliding scale clinics, and community health centers that offer affordable care. For example, organizations like the Asthma and Allergy Foundation of America (AAFA) provide comprehensive lists of resources, including local support groups and financial assistance opportunities tailored to individuals with allergies.
Another significant benefit of these groups is the emotional support they provide. Living with allergies can be isolating, and knowing that others understand your struggles can alleviate feelings of anxiety and frustration. The bonds formed in these settings often lead to lasting friendships and a sense of community, which can be essential for mental well-being.
- Networking Opportunities: Connecting with healthcare professionals and other patients can lead to better care.
- Resource Sharing: Members often exchange tips on managing symptoms and finding affordable treatments.
- Emotional Support: Sharing experiences can foster a sense of belonging and reduce feelings of isolation.
In conclusion, local support groups are an invaluable resource for patients seeking affordable allergy care. By connecting with others, patients can access a wealth of information, share experiences, and find emotional support, ultimately leading to better management of their allergies. As the landscape of healthcare continues to evolve, these community-driven resources remain a steadfast pillar in navigating the complexities of allergy treatment.
Community Workshops and Seminars
Community workshops and seminars are invaluable resources for individuals seeking to understand and manage allergies more effectively. These educational events, often organized by local health organizations, provide a platform for patients to learn about various aspects of allergies, from their underlying mechanisms to practical management strategies. Such initiatives not only enhance awareness but also empower individuals to make informed decisions regarding their health.
For instance, workshops typically cover a broad range of topics, including identification of allergens, symptom management, and treatment options. Participants might learn about common triggers such as pollen, pet dander, and certain foods, along with strategies to minimize exposure. According to a study published in the Journal of Allergy and Clinical Immunology, educational interventions significantly improve patients’ knowledge and self-management skills, leading to better health outcomes.
Moreover, these workshops often feature expert speakers, including allergists and immunologists, who share the latest research findings and treatment advancements. For example, recent studies have highlighted the effectiveness of immunotherapy in reducing allergic reactions over time. By attending these seminars, patients can gain insights into emerging therapies and evidence-based practices that may not be widely known.
Another critical aspect of these events is the opportunity for participants to engage in discussions and ask questions. This interactive format fosters a sense of community and support, allowing individuals to share their experiences and coping strategies. Research indicates that peer support can significantly enhance adherence to treatment plans, as individuals feel less isolated in their struggles.
In addition to educational content, workshops often provide information about navigating healthcare systems and accessing available resources. Many local health organizations partner with nonprofit groups to offer financial assistance programs, making allergy care more accessible. Participants can learn about sliding scale fees, community health centers, and insurance coverage options, which are essential for managing healthcare costs.
| Workshop Topics | Expected Outcomes |
|---|---|
| Identifying Allergens | Improved awareness of personal triggers |
| Symptom Management | Enhanced self-management skills |
| Latest Treatment Options | Knowledge of current therapies |
| Navigating Healthcare Resources | Access to financial assistance and care options |
In conclusion, community workshops and seminars serve as essential educational platforms that not only enhance patients’ understanding of allergies but also provide practical tools for effective management. By participating in these programs, individuals can improve their health literacy, connect with healthcare professionals, and access resources that facilitate better allergy care. This proactive approach ultimately leads to improved quality of life for those affected by allergic conditions.
Nonprofit Organizations
play a vital role in promoting allergy awareness and providing essential support to individuals facing the challenges of allergic conditions. These organizations not only advocate for better understanding and treatment of allergies but also offer financial assistance programs to help patients access necessary treatments without the burden of overwhelming costs.
Financial assistance programs provided by nonprofits can significantly alleviate the financial strain associated with allergy management. For instance, organizations like the Asthma and Allergy Foundation of America (AAFA) offer resources that connect patients with grants and subsidies designed specifically for allergy-related treatments. These programs can cover costs for medications, allergy testing, and even immunotherapy sessions, ensuring that patients receive the care they need.
Moreover, many nonprofits collaborate with healthcare providers to create community outreach initiatives. These initiatives often include free or low-cost allergy screening events, educational workshops, and informational seminars that empower patients with knowledge about managing their allergies effectively. For example, the Food Allergy Research & Education (FARE) organization frequently hosts community events to raise awareness about food allergies and provide practical resources for affected families.
In addition to direct financial support, nonprofits also serve as a bridge between patients and healthcare resources. They often maintain databases of local clinics and specialists that offer affordable care options. This is particularly beneficial for individuals who may be unaware of sliding scale clinics or community health centers that provide services based on income. For example, the Allergy & Asthma Network has a comprehensive directory that helps patients find nearby clinics that accept various insurance plans, including Medicaid and Medicare.
Furthermore, these organizations are instrumental in advocating for policy changes that benefit patients with allergies. By lobbying for increased funding for allergy research and better insurance coverage for treatments, nonprofits work to ensure that individuals with allergies are not left behind in the healthcare system. Their efforts can lead to significant changes that improve access to care and reduce the financial burden on patients.
In conclusion, nonprofit organizations dedicated to allergy awareness are invaluable resources for patients. Through their financial assistance programs, educational initiatives, and advocacy efforts, they help ensure that individuals can access the treatments they need without facing crippling costs. By connecting patients with vital resources and support, these organizations contribute significantly to improving the quality of life for those affected by allergies.

Conclusion: Making Informed Choices
In the complex realm of allergy and immunology care, making informed choices is essential for patients seeking effective and affordable treatment. As allergies can significantly impact quality of life, understanding the available options and resources is crucial for navigating this healthcare landscape. Awareness of various treatment modalities, financial assistance programs, and community support systems can empower patients to take control of their health.
Allergies manifest as abnormal immune responses to specific triggers, ranging from pollen to food. The field of immunology focuses on understanding these responses and finding ways to manage them effectively. Patients are encouraged to educate themselves about the range of treatment options available, which include medications, immunotherapy, and alternative treatments.
Medications, such as antihistamines, are commonly prescribed to alleviate symptoms. These can be obtained in both brand-name and generic forms, with the latter often providing a more cost-effective solution. For patients considering long-term treatment, immunotherapy—which involves gradually desensitizing the immune system to allergens—may be a worthwhile investment despite higher initial costs. Research indicates that patients who undergo immunotherapy experience significant symptom relief over time, ultimately reducing the need for medications.
In addition to traditional treatments, some patients explore alternative therapies, including acupuncture and herbal remedies. While these may offer relief, it is vital to consult healthcare professionals to ensure safety and efficacy. A study published in the Journal of Allergy and Clinical Immunology highlights the importance of evidence-based approaches when considering alternative treatments.
Finding affordable care requires proactive measures. Community health centers often provide sliding scale fees based on income, making them accessible to low-income patients. Furthermore, understanding insurance coverage is vital; patients should verify which services are covered under their plans to avoid unexpected costs. According to a report from the American Academy of Allergy, Asthma, and Immunology, utilizing in-network providers can lead to substantial savings.
Leveraging online resources is another effective strategy. Websites that compare clinic prices and patient reviews can guide individuals toward reputable providers. Telemedicine has also emerged as a valuable option, offering remote consultations at reduced costs—making specialized care more accessible.
Moreover, local support groups can serve as a wealth of information, providing patients with shared experiences and recommendations. Workshops hosted by health organizations often cover essential topics related to allergy management, enhancing community knowledge and support.
In conclusion, navigating the landscape of allergy and immunology care necessitates a proactive and informed approach. By utilizing available resources, understanding treatment options, and engaging with community support, patients can secure affordable care tailored to their individual needs. Empowering oneself with knowledge ultimately leads to better health outcomes and improved quality of life.
Frequently Asked Questions
- What are the common symptoms of allergies?
Allergies can cause a variety of symptoms, including sneezing, itching, nasal congestion, and skin rashes. Some people might also experience more severe reactions like difficulty breathing or anaphylaxis, which requires immediate medical attention.
- How can I find affordable allergy treatment options?
Finding affordable allergy treatments involves researching local clinics, checking community health centers, and looking for sliding scale fee structures. Don’t forget to explore online resources and patient reviews to identify the best options for your budget.
- Are over-the-counter allergy medications effective?
Yes, many over-the-counter allergy medications, like antihistamines and decongestants, can be effective for managing mild to moderate allergy symptoms. Generic versions are often more affordable and can provide similar relief as brand-name drugs.
- What is immunotherapy, and how does it work?
Immunotherapy is a treatment option that gradually desensitizes patients to allergens. This can be done through allergy shots or sublingual tablets. While it may involve higher initial costs, the long-term benefits can lead to reduced symptoms and less reliance on medications.
- Does insurance cover allergy treatments?
Insurance coverage for allergy treatments varies significantly by plan. It’s essential to check whether your provider is in-network and understand your policy’s requirements for pre-approval or referrals to avoid unexpected costs.
- What role do community support groups play in managing allergies?
Community support groups can provide valuable information, resources, and emotional support for individuals dealing with allergies. They often share experiences, tips, and recommendations, helping members navigate their treatment options more effectively.